Summary
Jasmine D., a pseudonym, is a 21-year-old student in Birmingham, Alabama, who was recently treated for chlamydia, a common sexually transmitted infection (STI). It is preventable and treatable. Left untreated though, it can lead to serious reproductive health complications for women, including infertility. Jasmine believes that had she received comprehensive information on her sexual health—including information on protection from STIs, such as condoms—she could have made safer decisions to prevent being infected.
Instead, Jasmine received little information on her sexual health at school in Russell County. The main focus was on abstinence from sex. In middle school, she participated in a three-day abstinence education program that culminated with “promise rings” and an abstinence pledge. In high school, she learned the basics of anatomy and pregnancy in lessons that glossed over prevention and treatment of STIs and HIV. She told Human Rights Watch that she learned about STIs and protection only after she contracted chlamydia, but “at that point, it was just too late.” Wistfully, Jasmine reflected, “I believe if I were knowledgeable [about condoms and STIs], it would have prevented it.”
Comprehensive sexual health education could have had a positive impact on Jasmine’s health, making it less likely that she contracted an STI and more likely that she got testing and treatment earlier.
Alabama has high rates of STIs and related preventable diseases, including cancers associated with the human papillomavirus (HPV), such as cervical cancer, and sexual health education could have a tremendous impact in improving health outcomes of young people in the state. Human Rights Watch has underscored that the high rates of cervical cancer deaths in Alabama are not just a failure of public health, but a human rights failure. Cervical cancer is highly preventable and treatable. With medical advances in diagnostic and treatment services, no one should die of the disease, yet the National Cancer Institute estimates that about 4,300 women will die of cervical cancer in 2020—including 100 women in Alabama. This indicates a slight increase in mortality rates since 2017, when 4,207 women died of the disease, according to the latest data available from the Centers for Disease Control and Prevention (CDC). Mortality rates are higher for Black women, poor women, and those who lack access to health insurance. According to the CDC, in 2017 Alabama was among the top five states in the country in terms of the highest rate of cervical cancer cases and deaths. Black women in Alabama are nearly twice as likely to die of the disease as white women. Previous Human Rights Watch research from 2017 and 2018 explored the barriers preventing Black women in Alabama from receiving the reproductive health services necessary to prevent and treat cervical cancer.
In that research, Human Rights Watch found a combination of factors drive these poor outcomes in Alabama, including a shortage of gynecologists in rural areas, prohibitive transportation costs often required to travel to see a doctor for follow-up testing and treatment, and Alabama’s failure to expand Medicaid to increase healthcare coverage for poor and low-income individuals in the state. Human Rights Watch’s research also showed that without access to information, many women lacked the knowledge necessary to take steps to lower their risk of cervical cancer. These factors, among others, have left many Alabama women without access to lifesaving preventive and diagnostic services to lower their risk of cancer.
There are four key points of intervention where cervical cancer deaths can be prevented with appropriate laws, policies, and practices: through vaccination, screening, timely follow-up care after abnormal test results, and early treatment. Our research found that, as Jasmine’s case illustrates, lack of access to information on sexual and reproductive health during adolescence also creates barriers for women and girls to protect themselves, including information on HPV and the HPV vaccine, the importance of routine screenings, and where to go for low-cost and free reproductive healthcare services.
Although cervical cancer is believed by many to affect an older population, state investments in young people could lead to the near eradication of the disease. Yet Alabama is missing an opportunity to enact policies that could have a tremendous impact on the health outcomes of young people. All adolescents need access to comprehensive and accurate information on their sexual and reproductive health and rights, but many young people in Alabama are not receiving this critical information in school. Alabama has no mandate requiring sexual health education in schools. If schools do decide to teach sexual health education, the Alabama State Code requires a focus on abstinence. The State Code also contains stigmatizing language around same-sex activity and prohibits schools from teaching about sexual health in a way that is inclusive of lesbian, gay, bisexual and transgender (LGBT) youth. Alabama should be providing all adolescents with relevant and practical information on their sexual and reproductive health and on important steps they can take to protect themselves and lower their risk of adverse health outcomes throughout their lives, yet state policies that withhold and censor critical information on sexual and reproductive health in schools do the exact opposite.
In addition to failing to provide access to comprehensive, inclusive, and accurate information on sexual and reproductive health for all adolescents, Alabama is missing out on another critical intervention to address high rates of cervical cancer deaths through the HPV vaccine. Like education around sexual health, vaccinating adolescents against HPV at a young age could significantly lower the risk of cervical cancer and, if utilized widely, could possibly wipe out cervical cancer for future generations of young women. HPV also causes six HPV-related cancers that affect all genders, including cancers of the vulva, vagina, penis, anus, and oropharynx. The HPV vaccine is an effective cancer prevention tool and protects against most of the strains of HPV that can lead to cancer. To be most effective, however, it must be administered before individuals start sexual activity and are exposed to HPV.
Despite its tremendous potential to lower the risk of cancer, vaccination rates in Alabama are low. Schools in Alabama are not providing adolescents with critical information about HPV, including what it is, the role it plays in causing cancer, and steps that they can take to lower their chance of contracting the virus. A lack of accurate and comprehensive information about HPV hinders young people’s ability to make educated decisions and take steps to lower their risk of cancer and safeguard their health in the critical period of adolescence.
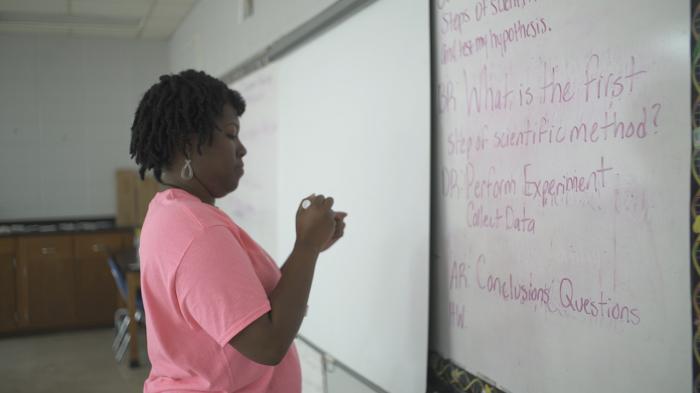
Between May 2019 and January 2020, Human Rights Watch interviewed 45 adolescents and young adults who attended schools in 16 counties in Alabama to learn more about their experiences with sexual health education and access to information on HPV and the HPV vaccine. Interviewees described the information they received in school and how this information, as well as gaps in their knowledge, had impacted decisions they had made affecting their sexual and reproductive health. Human Rights Watch also spoke with community members, academics, medical professionals, public health officials, and members of nongovernmental health, rights, and justice groups to better understand the current state of sexual and reproductive health in Alabama and how access to information impacts the health of young people.
This research found that Alabama is failing to educate young people about their sexual and reproductive health, despite the impact that access to this critical information can have on ensuring positive health outcomes into adulthood. Instead of providing students with knowledge and practical skills to make informed and safer decisions about their health, many schools in Alabama educate students only on abstinence. Abstinence-focused education programs that withhold critical information and shame sexuality are not only ineffective, but can be harmful. Many young people in Alabama described how abstinence-focused education stigmatized sexuality and made them reluctant to openly discuss their health concerns or seek out trusted sources of information. LGBT students, who typically are not provided with information that is relevant to them or a safe environment to explore their identities and concerns in schools, face even greater challenges in accessing information to make safer decisions on their sexual and reproductive health.
Young people in Alabama have a right to information to improve their health outcomes, yet state policies fail to ensure they receive this information. Without a state mandate on sexual health education, local school districts may decide whether or not to provide it. Misunderstandings about what sexual health content teachers are permitted to teach, as well as inadequate teacher training on sexual health topics, further limits the effectiveness of instruction on sexual health. Inadequate funding leaves certain school districts, particularly in rural and less wealthy regions of the state, unable to provide students with sexual health education, creating inequalities in access to information. This unequal access can create lifelong disadvantages for certain students, particularly those who are poor and Black, and may contribute to racial disparities in health outcomes as they age into adulthood.
Against the backdrop of this general failure to educate young people about sexual and reproductive health, schools are also not providing adolescents with lifesaving information to prevent HPV and lower their risk of cancer. Since more than 80 percent of individuals in the United States will eventually acquire HPV, sexual health education can be instrumental in educating young people about safer sexual practices to lower their risk of cancer, including cervical cancer. Yet schools are not educating adolescents around HPV, the HPV vaccine, and steps they can take to protect themselves from the virus. Various barriers, including stigma and parental opposition to a vaccine associated with sexual activity, ineffective recommendations from medical providers for the vaccine, and an inadequate number of vaccine providers in Alabama, contribute to low vaccination rates.
All adolescents in Alabama have the right to the highest attainable standard of health, and information is necessary for them to realize this right. By failing to mandate comprehensive sexual health education, Alabama is missing out on a critical opportunity to lay the foundation to improve health outcomes for young people. This is especially important in a state with poor health outcomes and high rates of STIs and HPV-related cancers. Alabama should enact legislation mandating comprehensive sexual health education in all primary and secondary schools that is age-appropriate, scientifically and medically accurate, rights-based, and inclusive of all young people in the state. Sexual health education should be incorporated into the curriculum and reach students from an early age, building incrementally to equip them with developmentally relevant information about their health and well-being. The state should also adopt clear policies that facilitate education around HPV and the HPV vaccine as an effective cancer prevention tool to increase vaccination rates. Until all adolescents in Alabama have access to comprehensive information to make informed decisions, protect themselves, and lower their risk of HPV and other STIs—as well as access to preventive tools like the HPV vaccine—they will continue to face a high risk of preventable diseases, like cervical cancer, and poor health outcomes.
Recommendations
To the Alabama State Legislature:
- Adopt legislation to support comprehensive sexual health education in Alabama. Legislation should:
- Mandate comprehensive sexual health education in Alabama schools that is age-appropriate, scientifically and medically accurate, and responsive to the needs of all young people. Such education should provide adolescents with developmentally appropriate information on their health and well-being, as well as practical information on how to lower their risk of unintended pregnancies and STIs, including HPV.
- At a minimum, update the State Code to ensure medical accuracy and remove the focus on abstinence and stigmatizing language around same-sex activity; support implementation of an updated State Code.
- Enact legislation to support an increase in HPV vaccination rates in Alabama. Legislation should:
- Require vaccines to be entered into the Immunization Patient Registry with Integrated Technology (ImmPRINT).
- Disseminate information on Advisory Committee on Immunization Practices (ACIP)-recommended adolescent vaccines to the parents or guardians of all students in Alabama completing the 5th grade.
- Require education around HPV for all students starting in 6th grade.
- Allocate funding to community-based organizations for public awareness and outreach campaigns around HPV and the HPV vaccine.
- Require all health insurance plans for residents of Alabama to provide coverage for the HPV vaccine for both men and women up to age 45, in accordance with US Food and Drug Administration guidelines; information on eligibility for the vaccine should be easily accessible and disseminated widely.
- Allocate funding to cover the cost of administrative fees for Vaccines for Children (VFC) providers to support an increase in the number of VFC providers in Alabama.
- Appropriate funds for comprehensive sexual health education in all primary and secondary schools in Alabama.
- Reform Alabama’s school financing system to ensure funding is targeted to increase state investment in schools in underserved communities.
- Adopt legislation to expand Medicaid under the Patient Protection and Affordable Care Act to increase access to medical services for Alabama residents.
- Appropriate sufficient funds for cervical cancer prevention, treatment, and maintenance care.
To the Governor of Alabama:
- Support revisions to the State Code that remove the focus on abstinence and ensure sexual health education is comprehensive, medically and scientifically accurate, and inclusive of all students.
- Create and launch a rights-respecting and youth-centered plan to increase HPV vaccination rates in the state.
- Develop a comprehensive, rights-respecting plan to eliminate cervical cancer deaths in Alabama and work with the state legislature to fund it.
- Support the expansion of Medicaid under the Patient Protection and Affordable Care Act to increase access to medical services for Alabama residents.
To the Alabama State Department of Education:
- Develop and circulate a model curriculum on sexual health education for schools to follow that is comprehensive, medically and scientifically accurate, and inclusive of all students. The curriculum should be based on national and international sexual health education standards and include information on how to obtain and use different methods of contraception.
- Update the 2019 Health Course of Study to ensure anchor and content standards include sexual and reproductive health and HPV.
- Create and implement methods for tracking the content of sexual health education curricula of all Alabama school districts, requiring schools to report annually to the Alabama State Department of Education on their instructional materials, instructional time per grade, and methods of assessing students’ knowledge on sexual health.
- Require certification and annual training on sexual health for all health teachers. Training should include: the most recent medical information on HIV and STIs; how to obtain and use methods of contraception; pregnancy; healthy relationships; human sexuality; and how to create a learning environment that is safe and inclusive of all students.
To Alabama School Administrators:
- Adopt clear policies on, and offer, comprehensive sexual health education that is age-appropriate, medically and scientifically accurate, and inclusive of all students; these policies should be informed by the needs of young people and created in collaboration with community members, including adolescents, to address specific community health concerns.
- Provide a model curriculum on sexual health education for health teachers, as well as training on content, effective instruction, and methods of assessing students’ knowledge on sexual health.
- Conduct trainings to ensure health teachers fully understand the State Code and local policies on sexual health education.
- Remove stigmatizing or degrading language around sexuality and sexual health in curricular materials.
- Provide students with access to accurate information and resources on their sexual health, including information on where to obtain accessible reproductive and sexual health services and products.
- Provide information on HPV and the HPV vaccine to parents and guardians.
To the Alabama Department of Public Health:
- To County Health Departments:
- In collaboration with local communities, conduct public awareness campaigns to build understanding of the HPV vaccine and disseminate information on the VFC Program, including eligibility requirements and locations where vaccines are administered.
- Partner with local communities, groups, and organizations to implement community-based initiatives to educate adolescents, including those who are out of school, on healthy sexual behaviors and to address stigma around sexual health.
- Protect the confidentiality of all patients, including adolescents who are sexually active, and ensure quality and comprehensive adolescent health services are provided by qualified medical personnel.
- Ensure reproductive health and cervical cancer resources are available and accessible in areas of the state where there is little access to reproductive health care. Appropriate resources for targeted outreach to communities so that residents fully understand cervical cancer prevention and how to access services to reduce cervical cancer risk through county health departments and state programs.
To the Alabama State Board of Medical Examiners:
- Conduct trainings for medical providers to improve the quality and effectiveness of recommendations for the HPV vaccine and ensure all providers understand that it is the standard of care to vaccinate against HPV; these trainings should convey how to effectively recommend the vaccine to parents and guardians and the need to recommend the vaccine for every child in the same way as all other recommended childhood vaccines.
To the US Congress:
- Adopt the Real Education for Healthy Youth Act or similar legislation to support comprehensive sexual health education and restrict funding to health education programs that are medically inaccurate or unresponsive to the needs of all students, including LGBT youth.
- Adopt the Youth Access to Sexual Health Services Act or similar legislation to provide communities with funding to increase access to sexual and reproductive health care and services for marginalized young people.
- Stop funding abstinence-only education grants and ensure adequate funding for comprehensive sexual health education programs.
- Enact the Student Non-Discrimination Act or similar legislation to prohibit discrimination in schools on the basis of sexual orientation and gender identity.
- Pass legislation aimed at addressing high cervical cancer mortality rates, particularly for women of color.
- Support Medicaid expansion into all states to address preventable deaths from gynecological cancers.
- Appropriate funding to increase the number of VFC Program providers in areas where adolescent vaccination services are limited and to build awareness of the program and its services.
- Appropriate funding to reinstate the Breast and Cervical Cancer Early Detection and Control Advisory Committee.
Methodology
This report is based on interviews conducted by Human Rights Watch in May, June, July, and December 2019, and January 2020. Individual interviews were conducted with 45 adolescents and young adults between the ages of 14-26. Human Rights Watch interviewed: 6 adolescents under age 18; 20 people between the ages of 18-21, and 19 people between the ages 22 and 26. Interviews were conducted with young adults ages 22 to 26 in order to better understand how information learned in middle and high school has impacted their knowledge of and decisions around sexual and reproductive health into adulthood.
The majority of interviews took place in person in seven counties in Alabama: Jefferson, Macon, Madison, Mobile, Shelby, Tuscaloosa, and Wilcox counties. Twelve interviews were held over the phone. Interviewees shared their experiences of sexual health education from 16 counties in Alabama: Baldwin, Calhoun, Coffee, Crenshaw, Jefferson, Lauderdale, Lowndes, Macon, Madison, Marengo, Mobile, Montgomery, Russell, Shelby, St. Clair, and Wilcox counties.
Seven interviewees were currently in high school or had received a Graduate Equivalency Degree (GED) when interviewed. Of the 38 young people interviewed who had graduated from high school, 35 graduated from public high schools, including 4 who attended public specialty or magnet schools. Two interviewees attended private, religious high schools and one attended a private nonreligious school.
The majority of interviews were conducted with adolescent girls and young women since cervical cancer impacts individuals with a cervix. Human Rights Watch sought to interview individuals with different gender identities and sexual orientations to capture a range of experiences.[1] Most interviewees identify as female, but Human Rights Watch interviewed one male participant and two participants who identify as non-binary or genderqueer. Ten interviewees identify as LGBT or queer.[2]
Human Rights Watch also spoke with 41 community members through group interviews and discussions conducted in 3 counties in the Black Belt, a rural region of Alabama with a predominantly African American population, widespread poverty, and poor health outcomes, including Greene, Macon, and Wilcox counties. An additional group interview was held in Conecuh County. Two interviews were conducted with high school teachers in two Black Belt counties.
Human Rights Watch also interviewed or consulted with 27 academics, medical professionals, public health officials, and members of nongovernmental health, rights, and justice groups.
Review of secondary sources, including the State Code of Alabama, the 2019 Alabama Health Course of Study, and data from the Alabama Department of Public Health and the Centers for Disease Control and Prevention’s 2015 Youth Risk Behavior Survey (YRBS) and 2018 School Health Profiles, were also consulted in the analysis of findings presented in the report.
All interviewees were informed of the purpose of the interview, its voluntary nature, and the ways in which the information would be collected and used. Interviewers assured participants that they could end the interview at any time or decline to answer questions without negative consequences. All interviewees provided oral informed consent to participate in an interview. Human Rights Watch has used pseudonyms in this report when interviewees requested anonymity or it was necessary to protect confidentiality. Human Rights Watch did not provide anyone with compensation for participating in interviews. For some group interviews, light refreshments, such as water and snacks, were served.
All interviews were conducted in English. Interviewees were identified through collaboration with organizations and community-based organizers with connections to adolescent girls and young adults within their communities.
|
A Note on Terminology in the Report “Child” or “children” refers to anyone under the age of 18. “Adolescent” refers to individuals between the ages of 10 and 19, consistent with the definition used by the World Health Organization (WHO).[3] The term “youth” refers to the period of transition from childhood to adulthood, defined by the United Nations as those who are between the ages of 15 and 24.[4] In this report, the term “young people” is used to refer to persons between the ages of 14 and 26. “Comprehensive sexual health education” refers to education around sexual and reproductive health that is age-appropriate, medically and scientifically accurate, and inclusive of and responsive to the needs of all young people. It encompasses the seven topics that are considered the minimum, essential content and skills for education on sexual health for kindergarten through 12th grade as defined by the updated National Sex Education Standards: consent and healthy relationships; anatomy and physiology; puberty and adolescent sexual development; gender identity and expression; sexual orientation and identity; sexual health; and interpersonal violence.[5] Additional terminology to describe sexual health education, such as comprehensive sexuality education (CSE) and sex education, are used in this report when referencing specific sources. “Sexually transmitted infection” (STI) is used to define infections that are passed between individuals through sexual contact and is the preferred term in the report; “sexually transmitted disease” is used when referencing a specific source of information or quotation in which that exact terminology appears. |
I. Gaps in Sexual Health Education in Alabama
They make it seem so scary and so life or death, and it is if you’re uninformed, and then they don’t inform us.
—Chloe L., 21, Huntsville, June 2019
Schools play a vital role in providing youth with access to information, including on their sexual and reproductive health. According to the US Centers for Disease Control and Prevention (CDC), schools “can be instrumental in educating students about human immunodeficiency virus (HIV), sexually transmitted diseases (STDs), and unintended pregnancy prevention and can reduce adolescents’ health risks through delivery of effective health education.”[6] Despite the positive impact they can have on the health outcomes of youth, Alabama schools are failing to provide adolescents with access to accurate and comprehensive information about sexual health. Young people in the state are left with critical gaps in knowledge and information on their sexual health, which directly impact their ability to make decisions and take steps to protect themselves from unintended pregnancy, sexually transmitted infections (STIs), and other adverse health outcomes. State policies that withhold critical information on sexual and reproductive health from young people undermine their right to health and can lead to poor health outcomes into adulthood.
According to the 2018 School Health Profiles, a biennial survey conducted by the CDC that assesses policies and practices around health education in schools in the United States, about 95 percent of high schools in Alabama taught students the benefits of being abstinent and educated them on the transmission of HIV and other STDs, but approximately one-third of high schools did not teach students the importance of using a condom correctly and consistently.[7] Even fewer high schools taught students how to use condoms.[8] This data is consistent with findings from Human Rights Watch research: young people in Alabama may be educated on risks to their sexual health, but they often lack crucial information to take steps to actually protect themselves.
In a state where young people are at a high risk of STIs and HPV-related cancers, this lack of information can be life-threatening. Conversely, comprehensive sexual health education can play a vital role in equipping adolescents with the knowledge and skills they need to make safer and informed decisions on their sexual and reproductive health. It not only addresses the physical and biological aspects of sexuality, including risk-reduction and disease prevention, but also equips young people with the information they need to navigate and develop healthy relationships, explore their own identities, and make educated decisions as they mature into adulthood. Research shows that comprehensive sexual health education can positively influence the behaviors of young people, contributing to delayed initiation and decreased frequency of sexual intercourse, decreased number of sexual partners, increased use of condoms and other methods of contraception, and a reduction in sexual risk-taking behaviors.[9] Since many risk factors for cervical cancer are tied to sexual activity, comprehensive sexual health education that results in safer sex practices for young people can have an impact on cancer rates.[10] In the US, highly respected medical and public health organizations, including the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists (ACOG), and the American Public Health Association, have voiced support for comprehensive sexual health education.[11] The United Nations World Health Organization (WHO) considers sexual health education that is age-appropriate and culturally relevant to be a primary intervention against the transmission of STIs, including HPV.[12]
On the contrary, abstinence-only sexual health education programs that withhold critical information on sexual health, promote inaccurate information, and often ignore or stigmatize healthy adolescent sexual behaviors, and particularly lesbian, gay, bisexual and transgender (LGBT) youth, can be outright harmful to young people.[13] Evaluations of these programs have consistently shown that they are not effective.[14] The United Nations Educational, Scientific and Cultural Organization (UNESCO) has stated:
While abstinence is an important method of preventing pregnancy, STIs and HIV, CSE [comprehensive sexuality education] recognizes that abstinence is not a permanent condition in the lives of many young people, and that there is diversity in the way young people manage their sexual expression at various ages. Abstinence-only programmes have been found to be ineffective and potentially harmful to young people’s sexual and reproductive health and rights.[15]
It is estimated that since the mid-1990s, the US federal government has spent nearly US$2 billion in abstinence-only funding, yet a multitude of studies have found no effect on reducing rates of adolescent pregnancy or a lack of sufficient evidence to draw conclusions.[16] However, studies have found that comprehensive sexual health education, which includes both abstinence and safer sex, to be effective at promoting safer sexual behaviors, including delaying or reducing sexual activity and increasing the use of condoms and other forms of contraception.[17]
Despite the numerous benefits of comprehensive sexual health education and the positive impact it can have on the sexual behaviors of youth, Alabama does not mandate sexual health education. Schools can decide to offer sexual health education, but the Alabama State Code limits what information can be taught. The State Code mandates an emphasis on abstinence, and states that any school that teaches sexual health should emphasize that “Abstinence from sexual intercourse is the only completely effective protection against unwanted pregnancy, sexually transmitted diseases, and acquired immune deficiency syndrome (AIDS) when transmitted sexually.”[18] The emphasis on abstinence limits students’ ability, in particular those who are sexually active, to make informed and safer decisions about their sexual health.
The Alabama State Department of Education issues a framework for health education in grades kindergarten through 12. Most recently updated in 2019, this framework, known as the “Alabama Course of Study: Health Education” (Health Course of Study), includes the minimum content required for health education in schools as well as a breakdown of the skills and knowledge students should have at every grade level, with a focus on developing “health literate citizens.”[19] Within the Health Course of Study, health education is broken down into eight anchor standards that align with the CDC’s National Health Education Standards.[20] Each anchor standard includes content standards that are required to be taught.[21]
Despite not mandating sexual health education, a 1987 resolution adopted by the Alabama State Board of Education requires that all students in grades 5 through 12 learn about HIV and AIDS through a health education program.[22] Given this requirement, all students in Alabama schools should receive some form of education on this particular aspect of sexual health.
|
International Guidelines on Comprehensive Sexuality Education The United Nations “International Technical Guidance on Sexuality Education” is a framework based on international best practices to help develop, implement, and monitor comprehensive and effective sexual health education programs.[23] According to the guidelines, comprehensive sexuality education (CSE): is a curriculum-based process of teaching and learning about the cognitive, emotional, physical and social aspects of sexuality. It aims to equip children and young people with knowledge, skills, attitudes and values that will empower them to: realize their health, well-being and dignity; develop respectful social and sexual relationships; consider how their choices affect their own well-being and that of others; and, understand and ensure the protection of their rights throughout their lives.[24] Beyond providing information on human anatomy, reproduction, and disease prevention, CSE empowers young people to build healthy and respectful relationships. In accordance with the guidelines, comprehensive sexuality education programs should be: scientifically accurate; incremental; age- and developmentally-appropriate; curriculum-based; comprehensive; based on a human rights approach; based on gender equality; culturally relevant and context appropriate; transformative; and enable students to develop life skills needed to support healthy choices.[25] |
Sexual and Reproductive Health Among Young People in Alabama
Many young people in Alabama are having sex at an early age and are engaging in behaviors that put them at a higher risk of unintended pregnancy and STIs, including HPV. According to the most recent data available on Alabama from the 2015 Youth Risk Behavior Survey, a national survey conducted by the CDC that monitors 6 categories of health-related behaviors for youth, about 46 percent of high schoolers in Alabama have had sexual intercourse, compared with approximately 41 percent nationwide.[26] Adolescents in Alabama are also having sex at an early age, with almost 7 percent of high schoolers in the state having sex before age 13, compared with approximately 4 percent nationally.[27] Alabama also has a high rate of high school students who are sexually active, and those who are sexually active are less likely to use condoms or other methods to prevent pregnancy than the average high school student in the United States.[28] Almost 35 percent of high schoolers in Alabama were sexually active at the time of the 2015 survey, around 5 percentage points higher than the national average.[29] Of those who were sexually active, approximately 51 percent used a condom the last time they had sex, compared to almost 57 percent of high school students across the country who used a condom.[30] Almost 18 percent of high school students in Alabama did not use any method to prevent pregnancy the last time they had sex, compared to 14 percent of high school students nationwide.[31]
Alabama also has high rates of STIs, placing young people at an even greater risk of poor health outcomes. According to the CDC, in 2018 Alabama had the 4th highest rate of reported gonorrhea cases and the 15th highest rate of reported chlamydia cases among US states.[32] From 2014 until 2018, reported cases of syphilis more than doubled in Alabama.[33] In 2017, young adults in their 20s had the highest rate of new HIV infections in the state.[34] Alabama also has high rates of teen pregnancy, ranking 9th in the country in 2017.[35]
|
The National Sex Education Standards The National Sex Education Standards, updated in 2020, were developed by the Future of Sex Education (FoSE) Initiative, a partnership between Advocates for Youth, Answer, and SIECUS: Sex Ed for Social Change. It provides a framework for comprehensive sexual health education in the United States. Influenced by existing health education standards, including the CDC’s National Health Education Standards and Health Education Curriculum Analysis Tool (HECAT), it addresses both functional knowledge around sexuality and skills young people need to adopt healthy behaviors.[36] It “provide[s] clear, consistent, and straightforward guidance on the essential, minimum, core content and skills needed for sex education that is age-appropriate for students in grades K–12 to be effective.”[37] The standards focus on seven topics that are essential for helping young people build the skills they need to make informed decisions about their health: consent and healthy relationships; anatomy and physiology; puberty and adolescent sexual development; gender identity and expression; sexual orientation and identity; sexual health; and interpersonal violence. |
Young People in Alabama Lack Critical Information on Sexual and Reproductive Health
Although most of the young people with whom Human Rights Watch spoke reported receiving some form of sexual health education in school, for almost everyone interviewed, it was far from comprehensive and adequate. Instead of providing information that could inform safer practices and lead to healthy sexual behaviors, it left them prepared to make only one choice: saying yes or no to sex. Many young people told Human Rights Watch that the little information they did learn about their sexual health, mainly through abstinence-only education, left them totally unprepared to understand their bodies, prevent STIs, and engage in safer sexual behaviors and healthy relationships. Several young people said that they believe the information they received was intended simply to scare them into saying no to sex rather than taking steps to stay healthy. The impact of this approach often followed them into adulthood, they said.
In describing the sexual health education that she received in high school, Monique S., 22, recalled how “it was actively harmful and not at all useful or valid information.”[38] Guest speakers who were brought into her 9th grade health class used harmful metaphors and shameful language around sex. They also showed graphic photos of STIs. Monique described messaging around sex as a doomsday scenario: “This is gonorrhea. This is chlamydia. This is what it looks like on your genitals and face and stuff. And here are your chances of getting it if you have sex even once.”[39] Beyond abstinence, Monique and her peers were not provided with any information on how to prevent STIs or how to protect themselves and stay healthy into adulthood. She said the education she received on sexual health “wasn’t about providing accurate information. It was about scaring people.”[40]
Alix T., 24, described messaging about sexual health as “don’t have sex or you’re going to either get an STD or get pregnant.”[41] Sexual health was stigmatized, and beyond the basics of pregnancy and reproduction, Alix and her peers did not learn about their bodies, how to protect themselves, or where to go for health services. She told Human Rights Watch that “the hour class that we had once when I was 11 [wasn’t] going to carry me through my high school years.”[42] According to Patricia E., 25, the abstinence-only education in her high school led by a church-affiliated outside presenter “was very much fear based rather than informative.”[43] The presenter used metaphors to shame students who have sex before marriage and was “one step away from saying that you’re going to go to Hell if you do this [have sex before marriage].”[44] Patricia said the presenter spoke of STIs, showing graphic pictures for some, but didn’t educate students around prevention or treatment options. Even for students who opt to wait to have sex within marriage, the information received was insufficient to support lifelong sexual and reproductive health as there was no education about having safer sex.
Sky H., 20, who identifies as non-binary, was sexually active in high school and received little information on how to prevent STIs, information they would have liked to have. Sky learned nothing about safer sex and said that STIs were presented only to scare students with messaging like “you’re going to get a disease if you have sex before marriage” and “condoms aren’t going to help.”[45] Sky’s health teacher refused to answer questions about condoms and birth control when they came up, telling the class “we’re not going to talk about that because you're not supposed to use those.”[46] Ashley W., 22, described how the abstinence education she received during middle and high school was intended to scare students and did not provide access to relevant information. She recalled how in the 6th grade the physical education teacher led a session on HIV, AIDS, and other STIs in which the overall messaging was “don’t have sex or you’ll get AIDS.”[47] There was no information on protection, safe sex, or testing: “If anything, they [STIs] were just presented as something that was very scary and not something that could be prevented or treated with medical care.”[48]
According to Hannah S., 23, the sexual health education she received “wasn’t really safety, it was shame.”[49] During health class in 11th grade, an outside presenter came in to teach sexual health. The presenter told the students that she got cervical cancer because she had sex before marriage, but didn’t discuss ways to lower the risk of cervical cancer. She used harmful metaphors for sex, showed graphic photos of STIs as a scare tactic, and shamed young women with messages like “don’t be sluts, stay abstinent.”[50] Not only was the information Hannah learned not useful, she found it harmful, describing how long it took for her to unlearn what she was taught in school. Hannah was coming out as a lesbian in high school and did not understand protection, something that made her nervous. She recalled how she didn’t know much about her own body, her reproductive organs, and what it meant to be sexually healthy during high school.[51]
Schools are also failing to provide young people with critical information to lower their risk of cervical cancer and otherwise support lifelong sexual and reproductive health. In addition to information on HPV and the HPV vaccine, discussed in the next section, young people need to have information on the importance of routine screenings, such as Papanicolaou (Pap) and HPV tests, and timely follow-up care after abnormal test results, as well as resources on where to obtain reproductive health services. Most of the young people Human Rights Watch interviewed did not learn this information in school.
Michelle S., 25, recalled how little she learned about her sexual and reproductive health growing up. Even though prevention of STIs and pregnancy was briefly covered in middle and high school, she didn’t receive information on how to lower her risk of cervical cancer, including information on HPV, the HPV vaccine, and Pap and HPV tests.[52] When her mom informed her that it was time to go to the doctor’s office for a Pap test, Michelle had no clue what it was for.[53] No one had explained to her what a Pap test is nor the difference between normal or abnormal test results. Even at age 25, Michelle reports still not feeling knowledgeable about her sexual and reproductive health.
Barriers to Comprehensive Sexual Health Education in Alabama
Despite the lifelong health benefits of comprehensive sexual health education, Alabama does not provide all adolescents in schools with information on their sexual and reproductive health. Policies that leave decisions about sexual health up to local school boards and fail to hold schools accountable for providing sexual health education have made it impossible to determine when students do receive sexual health education, the content they are learning, and gaps in critical information. Many teachers in Alabama also lack a clear understanding of the sexual health content they are required or permitted to teach, or do not receive adequate training on sexual health topics to ensure instruction is effective. The lack of state funding to ensure all schools have the resources to institute sexual health education programs creates additional barriers for schools that are already underfunded and overstretched. Without state policies to support sexual health education for students in all schools, Alabama continues to miss an opportunity to provide young people with inclusive and necessary information on their health.
Lack of a Statewide Mandate on Sexual Health Education
Alabama law does not require comprehensive sexual health education, leaving the decision to offer such education up to local school boards. School districts have autonomy to decide which sexual health topics to teach, beyond those included in the Health Course of Study framework and in line with state law, and can develop and implement curricula for their schools.[54]
Health teachers in Alabama rely on either their relevant school district policy, if there is one, or the Health Course of Study to develop their curriculum on sexual health, yet the Health Course of Study includes very limited content on sexual health. The anchor standard for grades 9-12 on health promotion and disease prevention, topics that should cover healthy sexual practices and the prevention of STIs, does not include content standards related to sexual health.[55] The minimum content that schools must cover, absent any local policy on sexual health, is inadequate to provide adolescents with a solid foundation for understanding their sexual health and steps to take to protect themselves.
The updated 2019 Health Course of Study framework includes a position statement on local sexual education policies stating that, “It is highly recommended that local school systems develop and adopt a policy regarding the instruction of sex education content for their schools in accordance with laws, regulations, and resolutions in age- and content-appropriate contexts.”[56] Yet, it is unclear how many school districts in Alabama have adopted policies on sexual health education and whether the Alabama State Department of Education monitors school district policies and sexual health education curricula. Human Rights Watch has requested this information from the Alabama State Department of Education but at the time of writing, has not received a response. Without oversight of sexual health education policies in the state, it is impossible to know exactly what information students are learning and to pinpoint critical gaps in information on sexual and reproductive health.
Misunderstanding of the State Code on Sexual Health Education
Confusion around the State Code and what sexual health content can and should be taught in schools in Alabama leads many health teachers to focus solely on abstinence. The State Code mandates an emphasis on abstinence but also states that course materials and instruction on sexual education and sexually transmitted diseases should also include education around contraception.[57] In effect, if abstinence or HIV/AIDS education is taught in schools, as mandated by both the Health Course of Study and a state resolution, schools are also supposed to be teaching students about contraception.
Despite this, many educators are unsure about what they are permitted to teach when it comes to sexual health. Many believe they can only teach students about abstinence. According to Christina Clark Okarmus, executive director of the Alabama Campaign for Adolescent Sexual Health based in Montgomery, this has led to a climate of fear within schools where some teachers, afraid to break what they perceive as a school rule or a law, will not discuss with their students methods of contraception or STI prevention beyond remaining abstinent.[58]
Human Rights Watch spoke with a health science teacher at a high school in the Black Belt who described how everything she teaches is tied to abstinence. As a teacher in a district that has not adopted a sexual health education policy, she bases her curriculum on the Health Course of Study. The teacher said that the State Code significantly limits the information she can share with her students, and she must teach about abstinence as the only method to prevent HIV and STIs: “As far as going into details about how you get it [HIV] and all that, I have to always say abstinence is the way that you don't get it.”[59] She said she understood the State Code to only permit teaching about abstinence in school.
Chloe L., 21, said that her health teacher during her junior year of high school moved quickly through topics on sexual health saying, “It was like the teacher was trying to get done with the subject as quickly as possible.”[60] Chloe described her teacher’s approach to sexual health: “I don't want to say anything that's going to potentially get me in trouble, I'm not here to offend anybody, here's the anatomy, and we're done.”[61] Whether or not this is what the teacher felt, Chloe perceived his discomfort and uneasiness covering topics on sexual health and believed it contributed to an already uncomfortable setting.
The CDC’s 2018 School Health Profiles highlights how teachers are not receiving training to better understand policies on sexual health education. Health teachers in only 23 percent of secondary schools in Alabama received professional development on how to understand district or school board policies or curricula on sexual health education in the two years leading up to the survey, despite a majority of health teachers wanting to receive this training.[62] Human Rights Watch has requested information on professional development regarding sexual health education for health teachers from the Alabama State Department of Education but at the time of writing, has not received a response.
Teachers in Alabama Lack Professional Development on Sexual Health
Educators who are responsible for teaching sexual health education in Alabama do not consistently have access to resources and training to ensure instruction is effective, which is especially important given that almost one-third of secondary schools in Alabama do not have a lead health teacher, defined as “the person most knowledgeable about health education at the school,” who is certified to teach health education.[63] Students feel that impact directly, and for many, the negative impact follows them into adulthood.
Human Rights Watch spoke with several young people who attributed the poor sexual health education they received in school to teachers who were inadequately prepared to teach the subject. Anna R., 21, said that her health teacher in 10th grade was a former basketball coach who seemed uncomfortable teaching sexual health education.[64] She said he skipped the section on sexual health entirely, telling the class “you guys know what sex is.”[65] Dionte R., 20, described how her health teacher during her sophomore year of high school was also the football coach, and seemed uncomfortable talking about sexual health. STIs were barely discussed and as Dionte recalled, he just pointed to the page in the textbook that covered them and moved along.[66] Lucien H., who is 18 and identifies as genderqueer, recalled that they barely learned anything about sexual health during the health class they took junior year of high school. They associate this with the dismal job of their teacher, who put little effort into teaching topics on sexual health. Lucien described how the health teacher made the class watch a video and read from a textbook, which no one actually did.[67] Lucien said they left the class having learned very little about sexual health: “What I learned was basically just enough to say they [the teachers] taught a class and not enough to make sure that the people they’re teaching are knowledgeable.”[68]
Such accounts are consistent with data from the CDC showing gaps in adequate training for health teachers in Alabama. Data from the CDC’s 2018 School Health Profiles highlights how little guidance and training on sexual health teachers in Alabama receive, including on key issues related to sexual health. In the two years leading up to the survey, lead health teachers received professional development on HIV prevention in only 26 percent of secondary schools in Alabama, although HIV/AIDS education is mandated by the state.[69] Health teachers in a little more than 20 percent of secondary schools received professional development on STI prevention.[70] An overwhelming majority of lead health teachers in Alabama also did not receive professional development to strengthen their instructional practices around sexual health education, including training on instructional strategies and methods for assessing students’ knowledge and skills on sexual health.[71]
Ongoing professional development for health teachers is essential to ensure instruction around sexual health is effective and aligned with best teaching practices, updated information on public health, and international standards. With medical advancements and breakthroughs occurring regularly in the public health field, teachers need training and resources to pass on accurate and updated health information to students. The 2018 School Health Profiles highlights the importance of training for teachers who teach sexual health education:
Parallel to quality curricula is the requirement of ongoing professional development (PD) and training to those teaching sexual health education. Successful PD training has been shown to increase both the amount of time teachers spend on health topics and their self-efficacy toward current and future sexual health education instruction.[72]
Recognizing the important role of educators on the quality of sexual health education, the Sex Education Collaborative developed the Professional Learning Standards for Sex Education (the Standards) in 2018 to provide guidance to school administrators and educators around ongoing professional development needed to implement effective sexual health education programs.[73] The Standards underscore the need for ongoing training of educators around best practices, skills, and knowledge of sexual health content. According to the Standards, “Knowing the facts about all of the topics covered in sex education is an essential part of being an effective teacher.”[74] Knowledge of best practices related to sexual health education can also help educators chose the most effective strategies to teach content and cover sensitive topics.[75]
By failing to invest in adequate training for health teachers to inform and guide their instructional practices, Alabama limits how effective sexual health education, when taught, can be.
Schools Do Not Have Adequate Funding for Sexual Health Education
Schools in Alabama lack adequate funding generally, and for sexual health education in particular. State funding for education is provided through the Education Trust Fund, which is funded through taxes, the largest being the individual and corporate income tax and sales tax.[76] In a bill appropriating funding for public education through the Education Trust Fund for fiscal year 2019-2020, there were no line items to provide supplemental funding for sexual health education to schools in Alabama.[77] Local school districts in Alabama must raise funds for sexual health education programs if they decide to offer them, a significant challenge for those that are underfunded and lack critical resources.
Limitations on property taxes in Alabama, rooted in discrimination and inequality, hinder the ability of many rural school districts to raise revenue for their schools, particularly for programs that are not required, such as sexual health education. Alabama’s 1901 constitution placed a cap on state and local property tax rates, which have been used to maintain white supremacy and systems of inequality in the state. As an Alabama federal district court stated in 2004, it is “a vestige of discrimination inasmuch as the [state] constitutional provisions governing the taxation of property are traceable to, rooted in, and have their antecedents in an original segregative, discriminatory policy.”[78] The caps protected landowners, who were generally white, from having to provide adequate social services, such as education, to primarily poor and Black children.[79] Until 1971, Alabama county tax assessors undervalued property, particularly in rural areas, “primarily to prevent adequate funding for black schools.”[80]
As a result of amendments to the constitution, agriculture and forestry are taxed at lower rates than many other property classes in Alabama and are given special exceptions.[81] Since property taxes account for most local funding for public schools in Alabama, these tax exceptions have had a detrimental impact on school districts, particularly rural districts that are left without adequate funding for their schools.
Cuts to state funding for education over the past decade have also placed immense pressure on local school districts in Alabama. Local districts rely heavily on the state to help fund education. The US Census Bureau found that, in 2017, 55 percent of funding for education in Alabama came from the state and approximately 35 percent came from local funds.[82] A report from the Center on Budget and Policy Priorities found that, adjusting for inflation, total state general funding per student was 15 percent lower in the 2018 school year than in 2008 in Alabama, despite increases to funding per student that have occurred in the last few years.[83] Because local school districts rely so heavily upon state funding for education, “cuts to state funding generally force local school districts to scale back educational services, raise more revenue to cover the gap, or both.”[84] In this context, local school systems in Alabama, many of which are already underfunded, have struggled to find revenue to offset a decrease in state funds, with implications for educational services offered to students. When school districts struggle to allocate funds to cover required courses and student services, an optional program, such as sexual health education, is not a priority.
Alabama’s current school financing system does not ensure that adequate funding is allocated to high-needs districts throughout the state. A study conducted by APA Consulting for the Alabama State Department of Education in 2014 and 2015 found that the state’s education funding system is not equitable and has increasingly become more inequitable.[85] The study found that Alabama could do more to support schools in low-wealth areas and recommended the state adopt a weighted student-based funding model to help ensure that state support for education is aligned with the needs of individual school systems.[86] Reforms to education financing could provide much needed funding for and investment in underserved school districts and help offset the inequalities that Alabama’s property tax system creates for schools in marginalized and rural areas of the state.
Given Alabama’s school financing model and the discriminatory nature of its property taxes, a lack of state funding for sexual health education can lead to inequality in access to critical information. Students who attend schools in wealthier districts that can afford sexual health education programs can benefit from information that is not available to their peers in underfunded districts, including students in the Black Belt where HIV rates are the highest in the state.[87] All students have a right to information without discrimination, yet students in rural, underfunded districts often lack access to information to prevent STIs, including HPV, and to lower cervical cancer risk, which can lead to lifelong disparities in health outcomes. Adolescents who grow up without information about their sexual and reproductive health, and about how to protect themselves and how to access services and treatment, may be less likely to take steps to lower their risk of adverse health outcomes than their peers who did receive this important information. However, Alabama is not even tracking what sexual health content is being taught in schools despite the data that shows there are significant sexual and reproductive health concerns throughout the state. Without clear information on what sexual health education students receive and where there are massive gaps in information, the state is missing out on an opportunity to identify any possible correlations between poor health outcomes and health disparities for certain regions of the state with a lack of access to sexual health education. This data could be useful in targeting resources to improve health outcomes.
The Second Edition of the National Sex Education Standards highlights the impact discrimination, structural racism, and social determinants of health have on the health outcomes of young people.[88] According to the Standards, sexual health education:
Should acknowledge the role that structural and contextual factors—personal, interpersonal, social, economic, and cultural—play in shaping adolescents’ sexual motivations and behaviors, with the fundamental goal of removing economic-, racial-, ethnic-, gender-, sexual orientation-, and ability-related disparities in adolescent sexual health.[89]
The Standards recognize and address the role structural factors have upon adolescent sexual health and focus on how characteristics, including race and socioeconomic status, are related to inequalities in health outcomes.[90]
Lauryn H., 20, did not receive sexual health education in school. She described how unlike schools in wealthier parts of Mobile, where she believed there was funding available to cover elective classes like sexual health education, in less affluent sections of the city like where she grew up, schools did not have adequate funding for sexual health education: “I was very lucky in the school that I did go to because it was one of the better of the poorer schools so I had excellent teachers who taught me the fundamentals of history and English and things like that but there wasn’t really room for sex ed or anything like that.”[91] According to Lauryn, all students in Alabama deserve comprehensive sexual health education and schools need funding, earmarked specifically to provide it.
Lack of Information Negatively Impacts Behaviors and Health Outcomes
Several of the young people Human Rights Watch spoke with attributed adverse health outcomes and poor decisions around sexual health to a lack of accurate knowledge and information they wish they had received in school. Although many reported briefly discussing HIV and other STIs, they were not provided with useful information on how to actually prevent them or protect themselves, beyond not having sex. The sexual health education that Jasmine D., 21, received in school was primarily focused on abstinence, although she recalls briefly covering HIV and STIs in health class. She ended up contracting an STI and believes if she had received comprehensive information on her sexual health while in school, she could have made better decisions to prevent it:
From a result of me not having the knowledge, I did end up getting an STI. I believe if I were knowledgeable [about condoms and STIs], it would have prevented it. Thankfully, with medication and stuff, it wasn’t anything serious or long-term or chronic or anything like that. But I just learned about it after the fact, and at that point, it was just too late.[92]
Camille C., 21, said that sexual health was covered for only two days during her 9th grade health class and STIs and HIV were glossed over, without any meaningful discussion or education around contraception or methods of protection. She stated that “it wasn’t enough to…make good and informed decisions.”[93] Camille believes access to more comprehensive information could have impacted the decisions she made: “I feel like I could have made probably better decisions if I was more informed especially when it comes to [using] protection.”[94]
Without access to comprehensive and reliable information, young people do not have full and accurate information to make safer and informed decisions about their sexual and reproductive health. Beyond some discussion around healthy relationships, Anna R., 21, did not receive sexual health education in school and among her peers there was little information on contraception, the importance of prenatal care, or information on the full range of pregnancy options, including termination and adoption. She described how one of her friends was seeking ways to end a possible pregnancy but lacked information about safe abortion. The friend described to Anna how she was told by another classmate that if she got drunk and fell down a set of stairs, she could end the pregnancy, an option she was considering that could have put her health or even her life in danger.[95]
Camiya K., 21, said that it was only after she left high school that she learned of many resources that could have positively impacted her health, including free testing centers and female condoms. The heavy focus on abstinence in her school not only prevented her and her peers from taking advantage of these resources, but also fueled inaccurate and harmful beliefs around sexual behavior. One male peer in high school told her he didn’t want to use a condom, explaining to her that since he previously wore a condom “the lubrication from the condom would have still protected him.”[96] Another male friend, who was sexually active with another male, told Camiya he didn’t need to wear a condom because he couldn’t get his partner pregnant. A lack of information was deeply harmful to these young people who did not have an accurate understanding of the risks associated with unprotected sex and the steps they needed to take to protect themselves.[97]
Adolescents in Alabama Lack a Foundation for Healthy Relationships and Navigating Consent
Comprehensive sexual health education can lay the groundwork for educating young people around healthy relationships, navigating consent, and having often difficult conversations around protection. Many young people Human Rights Watch spoke with lacked access to information on healthy relationships in school, with several describing the adverse impact this had on their sexual behaviors and health. Less than one-third of the young people Human Rights Watch interviewed said that they had discussed healthy relationships while in school.
Joan A., 21, described how abstinence was always preached in school, especially to young girls, and she was never educated on protecting herself or having conversations with sexual partners about protection. Although she left for college believing she would wait until marriage to have sex, she ended up having unprotected sex with one person and contracted trichomoniasis, a common and treatable STI. She said that, “I didn’t have my own protection but I expected him to and he didn’t.”[98] Although she felt she should not have unprotected sex, Joan lacked not only the confidence to say no to her partner, but also an understanding of steps she could have taken to protect herself in that situation. She said:
I never really thought about me buying my own condoms. I thought … that the young man would have his own condoms. But now I know better, that you will have your own condoms because some young men, they don’t buy condoms and they prefer not to use them.[99]
Sky H. did not learn much about their sexual health while attending high school in a small, highly religious town. Sky was in an unhealthy relationship during high school which she says she didn’t realize at the time: “I did not recognize how unhealthy it was because there was no one that was able to discuss that with me, what a healthy relationship and sexual life looks like.”[100] Camiya K. said she didn’t realize until she was in college that there are other forms of abuse in a relationship beyond just physical abuse.[101] Comprehensive sexual health education can play an instrumental role in equipping young people with knowledge and skills to navigate challenging interactions and build healthy relationships with lasting impacts on health and well-being, yet many young people in Alabama are missing out on this crucial information.
Abstinence-only Education is Harmful
Many young people described how inadequate sexual health education, in addition to being ineffective, was deeply harmful. They said that abstinence-only programs stigmatized sex and sexual activity, scared youth, and shamed them into not discussing their sexual health or seeking out accurate information and resources on their health.
Ashley W., 22, who identifies as a gay woman, said the shameful messages that she received about sex and her sexual identity continue to impact her to this day. She said, “Every message that I ever got about sex, relationships, sexual health has all been wrapped in shame.”[102] She said that “it has carried with me into my adulthood and it’s something I am continuously trying to shake.”[103] At the age of 22, Ashley still has not been to see a gynecologist and she attributes this partly to the shame she felt around her sexuality growing up. Not only did Ashley’s school fail to educate her around sexual health, but the information she did receive had an adverse impact on the decisions she made around her reproductive health as an adult, leading her to forgo regular screenings and recommended well-woman visits with a gynecologist.
Anna C., 20, said the abstinence-only education she received during her junior year of high school was intended to scare students with harmful metaphors and stigmatizing language around sex. She recalled how the instructor, a nurse from an abstinence education network, held up a Snickers candy bar wrapper and compared it to a condom, asking the class if they believed it would prevent pregnancy. In another class, the instructor had boys in the class spit into a cup of water that she then compared to girls who have sex before marriage.[104] Anna said that the class was deeply harmful and many of her peers walked away thinking their sexuality was something to be ashamed of: “What did it do other than like freak us all out or make us scared to talk to anybody about sex or how to have healthy sex?”[105]
Although she was sexually active in high school, Ariel G., 23, said that she didn’t feel comfortable seeking out information or resources on her sexual health due to the shame she felt:
It [sex] was like seen as something so bad so I never felt like I wanted to speak up about it. Or if I wanted help, I never felt like I could reach out because I was already seen as a criminal for having sex. So, it makes it more like a kind of thing to be done in secrecy.[106]
Patricia E., 25, described how stigma around sex created barriers to accessing reproductive health services in her county. She said that, “anything sexual health orientated, birth control, even the HPV vaccine, anything that was geared towards women was really demonized.”[107] Although Patricia and her peers knew that they could access free resources and services, such as birth control and STI testing, at their county health department, they feared the stigma that could result from a trip there. Many of her peers lacked transportation and did not feel comfortable asking their parents to drive them to the county health department. They also feared that county health workers would not protect their confidentiality and would spread rumors back to the community on who went there for services and treatment. Stigma around sex also meant many young women in her town often relied solely on male partners for protection: “I remember as a girl if you went into a gas station or Walmart to get condoms, it’s a small town so everyone’s going to be looking at you.”[108] The shame young women felt around their sexual health, further reinforced by abstinence-only programs in school that stigmatized sexuality, had serious implications upon their ability to protect themselves and access reproductive health services.
Abstinence-only programs also leave youth with little information on their sexual health. On top of the stigma and shame they often feel, many young people in Alabama are left trying to find accurate information on their sexual health on their own. As Anna C. said, “It's almost like a coming of age, like [a rite of] passage for teenagers in Alabama to try and like put everything together, piece by piece.”[109]
Abstinence-only education provided Hazel T., 20, with little useful information on her sexual health. Without access to accurate information at school or at home, she turned to the internet for information. She realizes now that, without even a basic foundation for understanding her sexual health, the internet was not a safe and reliable source of information: “There’s no possible way to glean enough information from the internet, with no base to know what you need to be looking for, to really understand what is safe and what is not safe.”[110] The majority of young people Human Rights Watch spoke with reported turning to the internet or to their friends for this information, often leading to misinformation around sex and sexual health. Chloe L. said where she turned to for information on her sexual health was “100 percent the internet.”[111] Ashley W. said that she turned to the internet for information at a time when she “wanted a trusted source of information for myself.”[112] According to Abba M., 21, the vast majority of youth in Alabama are “getting their information about sex from the back of the bus, the internet, from movies.”[113]
Sexual Health Education in Alabama is Especially Harmful to LGBT Youth
In addition to the emphasis on abstinence, the Alabama State Code also includes medically inaccurate terminology and contains stigmatizing language and false information around same-sex activity.[114] It requires that course materials on sexual education or STIs include an “emphasis, in a factual manner and from a public health perspective, that homosexuality is not a lifestyle acceptable to the general public and that homosexual conduct is a criminal offense under the laws of the state.”[115] This information is inaccurate since the Supreme Court invalidated the law on criminal prohibitions on same-sex activity in private in 2003. The State Code also prevents sexual health education from being inclusive of all students, including LGBT youth. Alabama is one of six US states with laws restricting the discussion or “promotion” of homosexuality in certain school curricula, often referred to as “no promo homo” laws. Currently, legislative efforts to amend the State Code to remove stigmatizing language on same-sex activity and revise terminology on sexually transmitted infections and HIV/AIDS have not passed.[116]
The stigmatizing language is particularly harmful for LGBT youth in Alabama—prohibiting sexual health education that is inclusive of their health needs while promoting harmful messaging around same-sex activity within schools. It undermines their right to equality and non-discrimination and can lead to adverse health outcomes. According to research from the Gay, Lesbian and Straight Education Network (GLSEN):
LGBTQ students who attend school in states with a “no promo homo” law face more hostile school environments and have less access to the resources and supports that are crucial to their safety, well-being, and academic success, as compared to LGBTQ students in states without such laws.[117]
Human Rights Watch research in 2016 also found that LGBT students face bullying, exclusion, and discrimination in schools in Alabama and other states where policies fail to support LGBT youth.[118] Abstinence-only education, which reinforces the perspective that heterosexuality is the social norm, further shames and isolates LGBT youth.
Only two young people whom Human Rights Watch spoke with recalled discussing sexual orientation and gender identity in school. Several young people interviewed said it was not discussed in the least, not at all, or was absolutely not allowed in school, and one interviewee described it as “a forbidden topic.”[119]
Many young people told Human Rights Watch that the sexual health education they received in school stigmatized same-sex activity and created an uncomfortable learning environment for their LGBT peers. Anna C., 20, recalled that at the beginning of abstinence education, as her teacher was introducing the sexual health topics that students were going to cover with an outside instructor, he told the class that “homosexuality is a sin.”[120] Anna believed that her teacher felt compelled to say this, in line with the requirements of the State Code, and recalled this as being a very awkward moment within the classroom. According to Patricia E., the church-affiliated presenter who came in to teach abstinence-only education pushed heterosexuality and all information, including on STIs, was presented in a heterosexist way “assuming everyone would have relations with a man and a woman.”[121]
Young people told Human Rights Watch that sexual health education was not inclusive of the specific sexual health needs of LGBT or queer youth and failed to create any space for them to explore issues around their own sexuality and identity, at a critical time in their development. Lucien H. described how as a queer youth, the information they received on sexual health in school was far from inclusive. Lucien’s teacher did not cover any topic having to do with LGBT communities and when issues around LGBT communities came up in a video during health class, they were just ignored.[122] Stephanie C., 22, recalled how little information on sexual health she received at school and said that as a gay woman, access to information on her particular health needs was even more challenging. She said that information and resources on sexual health is lacking in schools: “I have to go out of my way to know these things [about her sexual health].”[123] She described how “there are things I just literally don’t know about,” and that it was difficult to get information. Even as a 22-year-old, Stephanie said that she still did not feel knowledgeable about her sexual health, and as a gay woman, accessing information and resources on her sexual health is “a whole different battle for me.”[124]
Hannah S., who was coming out as a lesbian in high school, described how she turned to the internet and sites like Tumblr, a microblogging platform where users can generate and post content, to learn more about her sexual health and sexual identity since she learned nothing about this in school.[125] Although Tumblr is a powerful platform for young people to connect with their peers and explore issues around gender and sexuality, because the content is user-generated, it is not possible to guarantee the scientific and medical accuracy of information being shared, which can further fuel misinformation around sexual health.
Young People in Alabama Desire Comprehensive Sexual Health Education
Young people in Alabama want access to comprehensive sexual health education. Every adolescent and young person who spoke to Human Rights Watch voiced support for education around sexual health that is comprehensive and facilitates access to information on their bodies and health. They see it as absolutely essential to making informed decisions to protect themselves and address issues, such as high rates of teen pregnancy and STIs, that impact their communities.
Destinee M., 17, said that sexual health education is necessary in her community where girls around her age are pregnant, but a lot of them “don’t know what’s happening to their bodies at all.”[126] She emphasized the important role that education could play in helping girls in her community better understand not only their bodies, but also how to prevent unintended pregnancy.[127] Chelsey W., 17, also spoke of the positive impact that sexual health education could have in her county, where rates of STIs are high. She believes that sexual health education and knowledge on STIs could help with prevention.[128] According to Shatavia P., 17, sexual health education is “important so that we [she and her peers] can protect ourselves, so that we can be healthy.”[129]
Crystal N., 25, said it was important to educate herself on sexual health since so few people in her community are educated. She described how little information her peers had on sexual health and recalled conversations with guys she has dated who didn’t believe they needed testing for STIs since they had only slept with a few women and didn’t have any outward signs of an infection or disease.[130] Crystal considers information on sexual health “as a form of protection,” and believes that “knowing what your risks are, knowing how things work, it can only protect you.”[131]
Michelle S., 25, said the messaging around sexual health in her community growing up was: “do not have sex because if you do you are at risk of getting an STI, an STD, or pregnant.”[132] She said, “That is the only thing that you hear.”[133] She believes that youth in her community need access to information that really educates them on their sexual health, versus receiving messaging that is meant to simply scare them into not having sex: “Instead of preaching, you know, and saying ‘no’, I think that there needs to be alternative ways to be taught prevention.”[134] To have a positive impact on youth, she considers it necessary to break the cycle of silence in her community where sexual health is not openly discussed.[135]
Research has shown that this is consistent with what adults also want for children in the US. Regardless of political affiliation, parents in the US overwhelmingly view sexual health education in middle and high school as important, and support the inclusion of a wide range of topics, such as STIs and birth control.[136] Adults in the US also overwhelmingly favor programs that do not just teach about abstinence, but also educate youth on additional methods of preventing pregnancy and the transmission of STIs.[137]
This is also true of parents in Alabama. In 2017, the University of South Alabama carried out a survey commissioned by the Alabama Campaign for Adolescent Sexual Health that found that a large majority of parents from diverse racial, educational, and socioeconomic backgrounds throughout the state support comprehensive sexual health education for their children in public schools.[138] Of parents surveyed, 83 percent believed that sexual health education should be taught in public schools in Alabama.[139] Most parents reported that it was very important to teach about methods to prevent HIV, AIDS, and other STIs in school.[140] Parents also overwhelmingly supported teaching about condoms and where to obtain methods of birth control, including condoms.[141]
II. Barriers to HPV Vaccine Uptake in Alabama
In addition to failing to provide all adolescents with information to make informed decisions about their sexual and reproductive health, Alabama is missing out on another critical intervention to address high rates of cervical cancer deaths through the human papillomavirus (HPV) vaccine. As with education around sexual health, vaccinating adolescents against HPV at a young age could significantly lower the risk of cervical cancer and, if used widely, could possibly wipe out cervical cancer for future generations of young women. Despite the impact this early intervention could have on health outcomes for all adolescents, HPV vaccination rates are low in Alabama.
The HPV vaccine is a proven method of preventing six HPV-related cancers that affect all genders, particularly when administered before the onset of sexual activity. HPV is the most common sexually transmitted infection (STI) in the US, with approximately 79 million Americans currently infected with the virus.[142] More than 80 percent of individuals in the United States will eventually acquire HPV.[143] According to the Centers for Disease Control and Prevention (CDC), HPV is so common that almost everyone who is sexually active and hasn’t been vaccinated will get it at some point in their lives.[144] Although most strains of HPV typically clear away on their own within two years, persistent infection with certain high-risk HPV strains can cause changes in cervical cells that can lead to cancer. Almost all cases of cervical cancer are caused by HPV.[145] HPV can also cause five other types of cancer including cancers of the vulva, vagina, penis, anus, and oropharynx which includes the back of the throat, tongue, and tonsils.[146] According to estimates from the CDC, in the US, HPV causes approximately 35,000 cases of cancer each year and it is responsible for approximately 90 percent of cervical and anal cancer cases, 70 percent of vulvar and vaginal cancers, and 60 percent of penile cancers.[147] Increasingly, oropharyngeal cancers are being linked to HPV with recent studies showing that about 70 percent of oropharyngeal cancer cases in the US are caused by HPV.[148] Historically, HPV has been associated with cervical cancer and females but males are also at risk. The number of cases of oropharyngeal cancers, which are more common in men, has been increasing each year and, in the US, it is now the most common HPV-related cancer, highlighting the need for more education and awareness of the vaccine as an important cancer prevention tool for both males and females.[149]
|
Cervical cancer is highly preventable and treatable. With medical advances in diagnostic and treatment services, no one should die of the disease, yet the National Cancer Institute estimates that about 4,300 women will die of cervical cancer in 2020—including 100 women in Alabama.[150] This indicates a slight increase in mortality rates since 2017, when 4,207 women died of the disease according to the latest data available from the Centers for Disease Control and Prevention.[151] |
Despite the instrumental role the HPV vaccine can play in preventing cancer, it is underutilized as a cancer prevention tool. Vaccination rates have remained low in the US, especially when compared with other recommended adolescent vaccines.[152] Only 50 percent of girls ages 13-17 have completed the recommended doses of the vaccine and vaccination rates are even lower for boys, with only 38 percent completing the series.[153]
Alabama Has High Rates of HPV-related Cancers yet Low Rates of the HPV Vaccine
Alabama suffers from high rates of HPV-related cancers, yet HPV vaccination rates across the state remain low. According to the CDC, in each year from 2011-2015, an estimated 555 cases of cancer in Alabama were likely caused by the HPV virus.[154] The Gardasil 9 vaccine could have prevented around 93 percent of these cases of cancer.[155]
Gardasil 9, the only HPV vaccine available in the United States, protects against the nine high-risk strains of HPV that cause 75 to 90 percent of cases of cervical cancer.[156] The CDC recommends two doses of the HPV vaccination for all adolescents ages 11 and 12, although the vaccine can be given to children as early as 9 years old.[157] For adolescents who start the vaccine when they are 15 or older, 3 doses of the vaccine are required.[158] In October 2018, the US Food and Drug Administration approved Gardasil 9 for all adults up to the age of 45, significantly expanding the pool of individuals who can now receive the vaccination.[159] Although the vaccine is most effective if given before the initiation of sexual activity, it can protect adults against new HPV infections that they have not already been exposed to.[160]
According to the latest data available from the CDC, in 2017 Alabama was among the top five states in the country in terms of the highest rate of cervical cancer cases and deaths.[161]
Alabama also tied Minnesota for the 10th highest incidence rate for oral cavity and pharynx cancers in the US.[162] Despite this, HPV vaccination rates in Alabama are low, falling behind national vaccination rates.[163] According to data from the CDC based on the 2017 National Immunization Survey–Teen, a national survey that monitors vaccination coverage among adolescents ages 13 to 17, Alabama ranked 41st in the United States for adolescent HPV vaccination rates and only 40 percent of adolescents ages 13 to 17 in Alabama were vaccinated against HPV, compared with almost 50 percent across the country.[164] Yet data from the Immunization Patient Registry With Internet Technology (ImmPRINT), the state reporting system used by the Alabama Department of Public Health, records HPV vaccination rates that are much lower. As of October 2017, around 40 percent of adolescents ages 13-17 in Alabama had started the HPV vaccine series, receiving at least one dose of the vaccine yet, only 24 percent had completed it, as registered in ImmPRINT.[165] Medical providers are currently not required to record adolescent vaccinations in the ImmPRINT system, creating a barrier to understanding true coverage rates in Alabama. Requiring registry in ImmPRINT for all vaccines, including the HPV vaccine, is an important step towards establishing accurate coverage rates and an understanding of barriers preventing widespread utilization of the vaccine throughout the state.
In addition to being below the national average, vaccination rates in Alabama are significantly below the Healthy People 2020 goal of having 80 percent of adolescents ages 13 to 15 vaccinated against HPV by 2020.[166] In a state with high rates of cancers related to HPV, such poor vaccination rates indicate a clear missed opportunity to combat preventable deaths.
Barriers to HPV Vaccination Uptake in Alabama
The HPV vaccine can have a tremendous impact on health outcomes in Alabama. However, several barriers have prevented it from being widely used as a method of preventing cancer in the state, including stigma associated with HPV as an STI. Many medical providers in the state fail to consistently and effectively recommend it to parents as a critical method of preventing cancer. Alabama does not have enough providers to administer the vaccine, including at no cost, to all eligible adolescents in the state. Alabama is also failing to educate parents and young people about HPV and the importance of the vaccine, preventing widespread awareness and acceptance of the vaccine as essential for adolescent health.
Stigma and Misunderstanding of HPV
Stigma around HPV as an STI has a detrimental impact on vaccination rates. Despite the crucial role the vaccine plays in preventing cancer, many parents continue to associate it primarily with sex and sexual activity.[167] According to Mary Anne King, the former executive director of the Laura Crandall Brown Foundation and former co-chair of the Alabama Adolescent Vaccination Task Force (AAVTF) Parent Education Committee, “for many people, information about the vaccine has been framed as associated with a sexually transmitted infection versus framing it as cancer prevention.”[168] Many parents who believe their children are not, or should not, be sexually active are reluctant to vaccinate them against a disease that is spread through sexual activity, with the belief that they aren’t at risk and the vaccine is not necessary. Most do not realize that the vaccine is designed to protect their children from the virus that causes various forms of cancer throughout their child’s lifetime.
Human Rights Watch spoke with several young people who described the impact stigma around sex had on their parents’ reluctance to vaccinate them against HPV. Ashley W., age 22, has not received the HPV vaccine. She said that her mother told her “you don’t need this” when her pediatrician recommended it during a visit. Her mother associated the vaccine with sexual activity and believed Ashley would not be at risk of contracting HPV.[169] Whitney M., age 22, said that her mother had adhered to all of the recommendations of her pediatrician when Whitney was growing up, including all adolescent vaccinations. When Whitney’s pediatrician recommended the HPV vaccine for her at age 12, her mother sternly refused, telling the doctor to never ask her about the vaccine again.[170] Whitney’s mother believed she should not be having sex and therefore didn’t need the vaccine.[171]
Due to the association with sexual activity, vaccinating adolescents against HPV can be perceived as condoning sexual activity, instead of preventing cancer. Jessica M., 24, grew up in a conservative town in Lowndes County. She described how in her community, “if you get that vaccine [HPV vaccine], it's like allowing you to have sex.”[172]
Research has shown that lack of parental understanding of the HPV vaccine is another barrier that influences parents’ decisions about vaccination.[173] One study found that 86 percent of parents surveyed in Alabama had misunderstandings about the vaccine, including several parents who did not know that it protects males as well as females.[174] Concerns about the safety of the vaccine also deter some parents when considering whether to vaccinate their children.[175] Outreach to parents and education about the HPV vaccine can play an instrumental role in addressing misconceptions, countering beliefs that the vaccine is not necessary, and ensuring that parents see it as an important method of preventing cancer for all adolescents.
Providers Fail to Consistently and Effectively Recommend the HPV Vaccine
Although not unique to Alabama, inconsistent and ineffective recommendations for the HPV vaccine from healthcare providers contribute to low vaccination rates. Research shows that an effective recommendation from a healthcare provider for the HPV vaccine has the most significant influence on vaccine uptake and vaccination rates are higher when parents receive a recommendation from a medical provider.[176] Despite the influence they exert, providers are not consistently recommending the vaccine in the same way that they do other adolescent vaccines, including tetanus, diphtheria, and pertussis (Tdap) and meningococcal, 2 vaccines routinely given to adolescents between 11 and 12 years old.[177] Studies have shown that providers are less likely to recommend the HPV vaccine if they are uncomfortable discussing sex with their patient’s parents.[178] According to the CDC, only 71 percent of parents of children 13 to 17 years in Alabama reported receiving a provider recommendation for the vaccine in 2018.[179] Only five states had a lower rate of provider recommendation for the vaccine.[180] Among those in Alabama whose providers recommended the vaccination, 74 percent of parents reported that their child received the vaccine.[181] For those who reported not receiving a recommendation, only 44 percent of parents reported that their child was vaccinated.[182]
When providers differentiate the vaccine from other recommended adolescent vaccines, present it to parents as optional, or fail to strongly recommend it, parents receive mixed messages on how important it really is.[183] Strong, presumptive recommendations that assume parents will vaccinate their children, focus on cancer prevention, and treat HPV as equally important as other required adolescent vaccines have proven to be an effective way of recommending the vaccine to parents.[184]
Strong provider recommendations for the HPV vaccine can have a tremendous impact on vaccination rates in Alabama. According to Dr. Jennifer Young Pierce, program leader of Cancer Control and Prevention at USA Health Mitchell Cancer Institute Mobile and the chair of the AAVTF Provider Education Committee, high HPV vaccination rates in some rural counties in Alabama can be tied to one or a few providers or clinics who have done quality improvement work to ensure that they are recommending the vaccine to parents and guardians in the most effective way possible.[185]
Many of the young people Human Rights Watch spoke with said that doctors or pediatricians either did not recommend the HPV vaccine or did so in a very neutral way. Jessica M. recalled how her pediatrician gave her mother a flyer on the vaccine and left the room so her mother could review it and decide whether or not Jessica would receive the vaccine. Although Jessica’s mother did decide to vaccinate her, her pediatrician did not strongly recommend it, did not frame it as a cancer prevention vaccine, and left her mother to make the decision by relying on the information she already knew about HPV or learned from the pamphlet, and not expert medical advice.[186] Before going to college, Hazel T., 20, had done research on HPV and knew she wanted to get the vaccine to protect herself. She told Human Rights Watch that her pediatrician, who her family had known for a very long time, was hesitant to bring up the vaccine due to its association with sexual activity and the potential that it might upset her mother. Instead of taking the lead and providing a strong recommendation for why it was important, Hazel’s pediatrician put the onus on her, waiting for Hazel to tell her mother she wanted to get vaccinated before chiming in with her medical recommendation.[187]
Most of the young people who spoke to Human Rights Watch who had completed the HPV vaccine pointed to the instrumental role their doctor played in recommending the vaccine and informing their parents that it was necessary. Many young people who had not been vaccinated could not recall if their doctor had recommended the vaccine or not.
Alabama Lacks Providers to Administer HPV Vaccines
Lack of access to providers for the HPV vaccine has been identified as a challenge to increasing vaccination rates, including in Alabama.[188] As of 2019, 20 counties in Alabama did not have a pediatrician.[189] Instead, a large percentage of pediatric care in Alabama is provided by family medicine doctors, including in many rural counties where there is no pediatrician. Studies have shown that family medicine doctors are less likely than pediatricians to strongly recommend the HPV vaccine, especially for adolescents ages 11 to 12.[190] Given the importance of strong provider recommendations, this can impact HPV vaccination rates. Clark County, one of the counties without a pediatrician, has the lowest HPV vaccination rate in the state, where only 7.4 percent of adolescents between the ages of 11 to 15 have received both recommended doses of the HPV vaccine.[191]
Free HPV vaccines in Alabama are administered through the Vaccines for Children (VFC) Program, a federal program that helps provide vaccinations recommended by the Advisory Committee on Immunization Practices (ACIP) to children whose parents or guardians cannot afford them.[192] Children under the age of 18 who are Medicaid-eligible, uninsured, underinsured, or American Indian and Alaska Native are all eligible for the VFC Program.[193] In addition to doctors, other healthcare providers including urgent care clinics, pharmacies, and school-based clinics can also participate as VFC providers.[194] However, there are not enough VFC providers in Alabama and in three of the counties in Alabama without pediatricians, the county health departments are the only VFC providers.[195]
There is no charge for vaccines administered by private and public healthcare providers enrolled in the program, however, there can be fees associated with administering the vaccine that must be excused if a family cannot afford it.[196] Funding to cover the financial loss providers incur when administrative fees are excused may offset some concerns providers have about enrolling in the program and help increase the number of VFC providers in the state.
Although the VFC program can fill gaps, it does come with challenges. To take advantage of services, parents and guardians need to have accurate and accessible information on the program, including eligibility requirements and information on where vaccines are offered. Lack of awareness of the VFC program and misconceptions about the program, including who is eligible for free vaccination services, can impact its goal of vaccinating underinsured and insured adolescents.[197]
Young People in Alabama Lack an Understanding of HPV and the Importance of the HPV Vaccine
Alabama is failing to provide young people with comprehensive and accurate information to make informed decisions to prevent HPV and lower their risk of cancer. Schools in Alabama are not teaching adolescents about HPV, the HPV vaccine, and steps that they can take to lower their chance of contracting the virus. Lack of accurate and accessible information hinders their ability to make educated decisions and take steps to safeguard their health at a critical time such as adolescence.
The majority of young people Human Rights Watch spoke with expressed a lack of understanding of HPV and the HPV vaccine. Although many reported having heard of HPV or seen commercials for the vaccine on television, the majority did not understand the role HPV plays in causing cancer and how the vaccine functions as a cancer prevention tool. Of the 45 young people Human Rights Watch interviewed, only 5 recalled having learned about HPV at all in school, with most reporting that it was covered only briefly when learning about STIs in health classes. Only three interviewees reported learning about the HPV vaccine in school.
Many interviewees who reported feeling quite knowledgeable about their reproductive and sexual health expressed gaps in their understanding of HPV and the vaccine. Abba M., 21, is active in a reproductive rights and justice organization at her college and has also taught community sexual health education for several years. She recalled that she barely learned anything about HPV in high school and it was not until she got to college and was exposed to HPV that she “had to do a bunch of googling” to try and understand the virus.[198] Even then, when she asked a friend for advice, she was told: “HPV isn't really a thing. You have it but you don't have it, so don't worry about it.”[199] Abba described to Human Rights Watch the confusion she shares with many of her peers around HPV:
It's really overwhelming because a lot of it [information] is really confusing and every time I asked someone about it, they gave me different information. I don't think anyone really understands anything about HPV. I've had multiple friends that like have had HPV, have been diagnosed with HPV, and I still don't think they really understand what it is.[200]
Patricia E., 25, said that the primary care doctors she saw as an adolescent in Marengo County did not recommend the HPV vaccine. She first heard about it when she saw a commercial on television when she was 17, but it was not until years later that she learned about the role the vaccine plays in preventing cancer: “I didn’t even know until I was 22 that the HPV vaccine was a preventive measure against cervical cancer.”[201] Although she ultimately did receive the vaccine, starting the series at the age of 23 when she visited a gynecologist for the first time, she missed the window during early adolescence when the vaccine is recommended and seen as most beneficial before any exposure to HPV. With access to information on the HPV vaccine and how it could protect her against cervical cancer, Patricia could have taken steps years earlier to lower any risk of ever contracting HPV.
Anna C., 20, said that HPV was briefly mentioned when covering STIs during the abstinence education class she took during her junior year of high school. She recalled that the only thing she learned about HPV was that “this is a thing you could get from sex.”[202] She said she did not learn anything about preventing or lowering her risk of contracting HPV, including information on the vaccine. Taylor P., 25, did not learn about HPV or the HPV vaccine in school. When she was 24, her Pap test came back abnormal and her gynecologist explained to her that she was at risk of HPV. Subsequent Pap tests came back clear however Taylor wished that she had learned about precautions to take to protect herself against HPV in school. With information on HPV, including the vaccine and how it prevents HPV, Taylor said: “I would have took the necessary precautions to not be at risk.”[203]
A lack of education around HPV also leads to misinformation about the virus and limits the ability of young people to educate their peers on this common and preventable infection. Although she received the vaccine, Michelle S., 25, admitted that even as a grown woman in her mid-twenties, she did not know much about HPV or the vaccine. She described confusion around how HPV is transmitted among her peers, with one friend believing that only men can catch the virus from women.[204] Jasmine D. said that although she didn’t learn anything about HPV in middle or high school, she felt she had learned more through her nursing classes and guest speakers who have lectured on sexual health. She now has a basic understanding of HPV but admitted that she would like to learn more about HPV and the vaccine so she can help educate other people, including her peers.[205]
Several of the young people Human Rights Watch interviewed could not recall if they had been vaccinated and a few believed they may have received an initial dose but were unsure. Fewer than half the young people interviewed could say for certain that they had completed the HPV vaccine series. The vaccine is only effective when all recommended doses have been completed, so an initial dose of the vaccine does not provide protection against HPV. Knowledge of the vaccine was low even among those who had received the vaccine and most reported that when they were vaccinated, they were not informed of the purpose of the vaccine and, at the time, many had no idea what it was for.
Crystal N., 25, completed the HPV vaccine, starting the vaccine series at age 14. She described how little information she was provided with at the time: “They basically said, ‘here’s your vaccine’ and stuck it in my arm. It’s not something that you generally hear about,” she said. “No one ever really talks about HPV.”[206] Hannah S., 23, said that she learned very little about HPV until she went to her first gynecologist appointment in college. When she started the vaccine series as an adolescent, she had no clue what it was for. She recalled how she was told, “It’s just for women’s health stuff.” Hannah knew she had received an initial dose of the vaccine but she wasn’t sure if she had finished it, describing this as a barrier to protecting herself.[207] With more information on the vaccine, Hannah could have advocated for herself, ensuring she completed the series and feeling confident that she had taken an important step towards lowering her risk of cancer in the future.
Efforts to Increase HPV Vaccination Rates in Alabama
The Alabama Department of Public Health (ADPH) currently leads the Alabama Adolescent Vaccination Task Force (AAVTF), which brings together diverse organizations, including those focused on health care, education, and advocacy, that are working towards increasing vaccination rates in the state, with a specific focus on the HPV vaccine.[208] In addition to national, regional, and statewide meetings to coordinate efforts, the AAVTF has undertaken efforts to raise awareness of the HPV vaccine through social media and billboard campaigns advocating for the vaccine throughout the state. The American Academy of Pediatrics and the AAVTF have also led a peer-to-peer mentoring program in which doctors mentor pediatricians to improve the quality of healthcare provider recommendations for the HPV vaccine.
The ADPH is currently working on a project to increase the number of VFC providers, including pharmacists and physician extenders, in counties where providers are limited to help boost vaccination coverage rates.[209]
Since 2006, at least 25 US states have implemented legislation to raise awareness of HPV and the vaccine by either: funding the vaccine, requiring the vaccine, or educating children in school or the public about the vaccine.[210] Currently, Alabama has not implemented any policy changes around HPV, despite high rates of cervical and oropharyngeal cancers.
To increase HPV vaccination rates, Alabama needs to enact legislation to educate the public and ensure that parents and adolescents in Alabama understand the importance of the HPV vaccine as an effective and lifesaving method of cancer prevention. The AAVTF is working on the Adolescent Vaccine Awareness Act, which would require schools to distribute information on the three recommended adolescent vaccines, including Tdap, HPV, and meningococcal, to parents and guardians of all students entering 6th and 7th grade. ADPH is also currently working on an ACIP School Rule Change, a policy change that would update current school vaccination requirements so all children entering daycare and kindergarten would need to receive all ACIP vaccines. When these children who are entering daycare and kindergarten reach adolescence, HPV will be required for school attendance. This policy change would have a tremendous impact on increasing future HPV vaccination rates by requiring it for school entry.
III. International Legal Standards
Alabama’s failure to ensure access to comprehensive, inclusive, and accurate information on sexual and reproductive health and to take steps to increase human papillomavirus (HPV) vaccination rates significantly undermines the health of young people. In failing to take critical steps to improve the health outcomes of all young people in the state, Alabama is also undermining fundamental rights related to and interdependent with sexual and reproductive health, including the rights to non-discrimination and information.
Right to Health
All people have the right to health, a principal established by numerous international instruments, including the Universal Declaration of Human Rights (UDHR), which all UN member states have endorsed and is broadly reflective of customary international law.[211] The International Covenant on Economic, Social and Cultural Rights (ICESCR) recognizes “the right of everyone to the enjoyment of the highest attainable standard of physical and mental health.”[212] The United States has signed but not ratified the ICESCR and is therefore not formally bound by its provisions, but it has the obligation to refrain from actions that would defeat the treaty’s object and purpose.[213] Many of the rights contained within the ICESCR are derived from customary international law. The right to health and the measures needed to uphold it, as enshrined in the ICESCR, extend beyond health care and is inclusive of underlying determinants of health, including access to education and information on sexual and reproductive health.[214]
The right to health also affords individuals the right to preventive care, and the ICESCR requires states to take steps to prevent and treat diseases.[215] According to the UN Committee on Economic, Social and Cultural Rights, fulfilling the right to health requires “the establishment of prevention and education programmes for behavior-related health concerns such as sexually transmitted diseases, in particular HIV/AIDS, and those adversely affecting sexual and reproductive health.”[216] The committee has also affirmed the need for states to develop and implement comprehensive strategies to promote women’s health with interventions aimed not only at treating, but also at preventing diseases that primarily affect women.[217]
Additionally, the Convention on the Rights of the Child (CRC), the primary instrument under international law that elaborates the rights of children, also affirms the right of all children to the highest attainable standard of health.[218] The United States has signed but not ratified the CRC, and is currently the only UN member state that is not a party to it. However, the CRC is an authoritative document for understanding the human rights of children, and the measures needed to effectively address them. The Committee on the Rights of the Child, the expert body that interprets human rights obligations set forth in the CRC, has recommended that states adopt age-appropriate, comprehensive, and inclusive sexual and reproductive health education as part of their mandatory school curriculum, with attention given to preventing STIs.[219]
The right to health is inseparable from the right to be free from discrimination, a protection included in the International Covenant on Civil and Political Rights (ICCPR).[220] The US ratified the ICCPR in 1992 and the US government is obligated to uphold the provisions of the covenant. Article 26 of the ICCPR states:
All persons are equal before the law and are entitled without any discrimination to the equal protection of the law. In this respect, the law shall prohibit any discrimination and guarantee to all persons equal and effective protection against discrimination on any ground such as race, colour, sex, language, religion, political or other opinion, national or social origin, property, birth or other status.[221]
The UN Human Rights Committee, which provides authoritative guidance on the ICCPR, has determined that this provision also prohibits discrimination on the basis of sexual orientation and gender identity.[222] The United States is obligated to protect LGBT students from discrimination on the basis of their sexuality or gender identity and to take steps to eradicate discrimination within schools.[223]
In its General Comment No. 14, the Committee on Economic, Social, and Cultural Rights underscored that the ICESCR prohibits discrimination in access to health care and underlying determinants of health on the basis of any status which “has the intention or effect of nullifying or impairing the equal enjoyment or exercise of the right to health,” including sexual orientation, social origin, or property.[224] The committee further noted that states have an obligation to prevent any discrimination, including discrimination that may not be overt, in respecting the core obligations of the right to health, including “education and access to information concerning the main health problems in the community, including methods of preventing and controlling them.”[225] The CRC also prohibits any form of discrimination against children and the Committee on the Rights of the Child has also concluded that unequal access to information on sexual and reproductive health amounts to discrimination, affirming that “all adolescents should have access to free, confidential, adolescent-responsive and nondiscriminatory sexual and reproductive health services, information and education.”[226]
The Committee on Economic, Social and Cultural Rights also notes the interdependence of the realization of the right to sexual and reproductive health, with the right to education and the right to non-discrimination and equality between men and women, which, when combined, entail “a right to education on sexuality and reproduction that is comprehensive, non-discriminatory, evidence-based, scientifically accurate and age appropriate.”[227]
Right to Information
The right to information is inseparable from the right to health. Although the right to health does not guarantee everyone the right to be healthy, it obligates governments to enact policies that promote accessibility to basic healthcare services, including accessibility to information on issues related to health, to everyone, without discrimination, especially for those who are most vulnerable and marginalized.[228] Policies in Alabama that fail to provide all students, including LGBT students and those from underfunded school districts, with equal access to information on sexual health undermine the right to health.
The right to information is enshrined in several human rights treaties. As part of the right to freedom of expression, article 19 of the ICCPR recognizes the “freedom to seek, receive and impart information and ideas of all kinds.”[229] This right to receive information is guaranteed to everyone, including young people. The ICESCR requires states to provide complete and accurate information necessary for the protection and promotion of rights, including the right to health.[230] In its General Comment No. 14, the Committee on Economic, Cultural and Social Rights states that, “States should refrain from limiting access to contraceptives and other means of maintaining sexual and reproductive health, from censoring, withholding or intentionally misrepresenting health-related information, including sexual education and information.”[231] The committee also affirmed that women’s right to health requires the removal of barriers that interfere with sexual and reproductive health, including education and information.[232]
The right to health also obliges states to share information that promotes healthy outcomes. The Committee on Economic, Social and Cultural Rights has determined that state obligations include “fostering recognition of factors favouring positive health results, e.g. research and provision of information” and “ensuring that the State meets its obligations in the dissemination of appropriate information relating to healthy lifestyles and nutrition, harmful traditional practices and the availability of services.”[233] The committee also determined that in deliberately withholding or misrepresenting information that is vital for protecting health, states violate their obligation to respect the right to health.[234] By not actively promoting science-based information on HPV and the HPV vaccine to parents and adolescents, Alabama is failing to provide access to information that could prevent adverse health outcomes, and possibly death, for individuals living in the state.
In General Comment No. 20, the Committee on the Rights of the Child concluded that all adolescents have the right to information on sexual and reproductive health, including on contraception, STIs, and safe abortion services: “All adolescents must have access to confidential adolescent-responsive and non-discriminatory reproductive and sexual health information and services, available both on and off-line.”[235]
The Committee on the Elimination of Discrimination against Women has similarly concluded that women’s right to health requires information on sexual and reproductive health. The committee further stressed the importance of access to information for all adolescents and the need for school-based education on sexual and reproductive health:
Furthermore, special attention is needed to ensure that adolescents have access to accurate information about their sexual and reproductive health and rights, including responsible sexual behaviour, prevention of early pregnancies and sexually transmitted diseases. Age-appropriate education on sexual and reproductive health should, therefore, be integrated in school curricula.[236]
Acknowledgements
This report was researched and written by Annerieke Daniel, fellow in the Women’s Rights Division at Human Rights Watch. Amanda Klasing, acting co-director in the Women’s Rights Division, provided additional research support. Brian Root, senior quantitative analyst in the Program Office, provided quantitative data analysis.
Amanda Klasing edited the report. Margaret Wurth, senior researcher in the Children’s Rights Division; Ryan Thoreson, researcher in the Lesbian, Gay, Bisexual, and Transgender Rights Program; Grace Meng, senior researcher in the United States Program; and Joe Amon, director of Global Health at Drexel University’s Dornsife School of Public Health, reviewed the report. James Ross, legal and policy director, provided legal review. Tom Porteous, deputy program director, provided program review.
Mary Olson, intern in the Women’s Rights Division, provided research support. Design and production assistance were provided by Erika Nguyen and Susanné Bergsten, coordinators in the Women’s Rights Division; Travis Carr, Publications and photographer coordinator, Fitzroy Hepkins, senior administrative manager; and Jose Martinez, senior administration coordinator.
We wish to thank the many reproductive health, rights, and justice groups, community organizations and advocates, academic researchers, and medical and public health professionals throughout Alabama who provided guidance and expert input. In particular, we would like to thank the following groups and individuals for their support: the Southern Rural Black Women’s Initiative (SRBWI); Christina Clark Okarmus (Alabama Campaign for Adolescent Sexual Health); Unite for Reproductive and Gender Equity (URGE); Dr. Jennifer Young Pierce (USA Health Mitchell Cancer Institute); Mary Anne King (formerly with the Laura Crandall Brown Foundation); and members of the Alabama Sexual Health Coalition and the Alabama Adolescent Vaccination Task Force.
Human Rights Watch is especially grateful to all the young people who shared their experiences and stories with us.